For years I’ve been saying this is the first platinum-based drug we discovered (Cisplatin). It can’t possibly be the best one. It’s disappointing that the scientific community has not been able to find better ones.
(Barnet Rosenberg 1926-2009)
Background
Designing new drugs with different molecular structures is one of the keys to treating the various types of cancer that kill over 8,000 people in Ireland, and 8 million people worldwide annually. Of the 16,000 cases reported in Ireland each year, only half of these survive, with lung and prostate cancer being the main causes of death through cancer on this island.
The precious metal platinum is used in a wide range of industries annually such as catalytic converters in cars, jewellery and some electronics. As well as these, approximately 1% of all the platinum produced each year is used for anti-cancer research.
In 1844 the Italian chemist Michele Peyrone reported the discovery of a chemical substance which would later become known as Peyrone’s Salt. The molecular structure of the salt was then determined by another chemist, Alfred Werner, in 1893, as part of his 1913 Nobel-Prize-winning work. However, it was not until 1965 that the biological activity of Peyrone’s Salt was discovered by the physicist Barnett Rosenberg of Michigan State University, at which time the substance then became known as cisplatin. Rosenberg initially discovered that by passing an electrical current through some platinum electrodes it generated a soluble substance. This substance turned out to be cisplatin, which he reported as affecting the growth of E. coli bacteria. The bacterial growth itself actually continued but cell division was stopped, resulting in long filaments of bacteria.
When confronted with these interesting research results, Rosenberg, as well as deciding to pursue them vigorously, also sought the help of other scientists outside his primary field. He enlisted the help and expertise of researchers trained in microbiology, inorganic chemistry, molecular biology, biochemistry, biophysics, physiology, and pharmacology. Cisplatin was subsequently introduced into clinical practice in 1971 and became one of the most successful anti-cancer drugs of all time with nearly 90% success rates against testicular cancer alone. It is still one of the most effective forms of treatment for certain types of cancer, such as non-small cell lung cancer (NSCLC), oesophageal (throat) cancer and ovarian cancer.
Cisplatin also started a whole new area of anti-cancer research based on platinum. Platinum-based drugs can induce death in cancer cells by the formation of chemical cross-links in DNA. All cells, both normal and cancerous, need DNA to replicate in order to multiply and survive. Platinum-based anti-cancer drugs act like throwing a spanner in this machine by preventing the DNA from replicating.
There are currently three platinum based anti-cancer drugs approved for clinical use world-wide: Cisplatin (1978), Carboplatin (1989) and Oxaliplatin (2002). Although these drugs have revolutionised cancer treatment, they have some very severe side-effects, including suppression of bone marrow activity and causing kidney problems, among others.
Research into finding new platinum-based anti-cancer drugs with less severe side-effects and increased potency is ongoing at various levels, from chemical coordination studies to cancer cell testing and clinical trials.
My project
All of the platinum-based drugs synthesised in my PhD project are designed to be stable, have minimum toxicity and to be effective against various cancer cells. Learning from over 50 years of platinum anti-cancer research, I successfully designed and synthesised 14 brand new platinum-based anti-cancer drugs. After various studies with bio-molecules commonly found in the body, such as Glutathione, I concentrated the rest of my studies on two of the best drugs, due to their solubility and ease of synthesis in the lab.
In order for anti-cancer drugs to make it to the manufacturing stage, they need to be easy to produce on a large scale; therefore, the design of new chemical drugs needs to incorporate how they are made. The two drugs I began concentrating on can be made in a “one-pot-synthesis”, which is almost unheard of for my particular type of platinum-based drugs, and makes them far easier to produce, should they get approved for clinical use.
Throughout the project the experimental procedures used to test the manufacturing of these drugs were completed on a very small scale, to ensure that the cost remains low. Most of the drugs produced were in a very pure form which is also essential for determining their activity towards cancer.
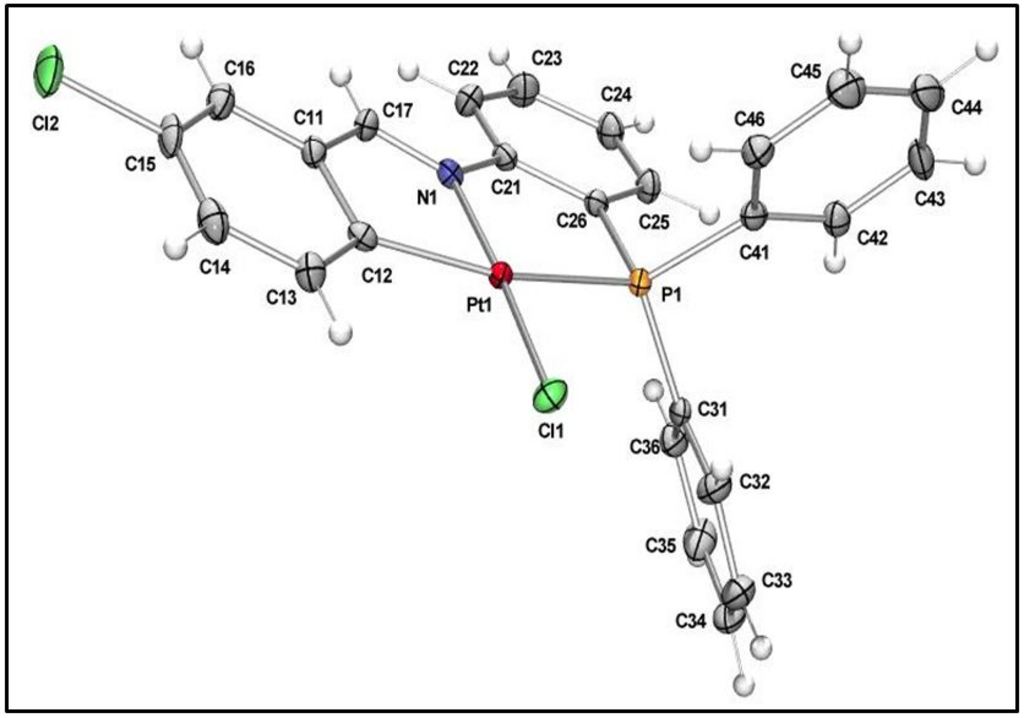
The drugs designed in this project, Figure 1, contain a platinum-carbon bond, which makes them much more stable and resistant to being attacked by bio-molecules within the body. Unfortunately the drugs were not soluble in water but some were quite soluble in ethanol and other organic solvents. The solubility of a drug is also very important for its success as many of them are given to patients in a solution by injection.
Testing on cancer cells
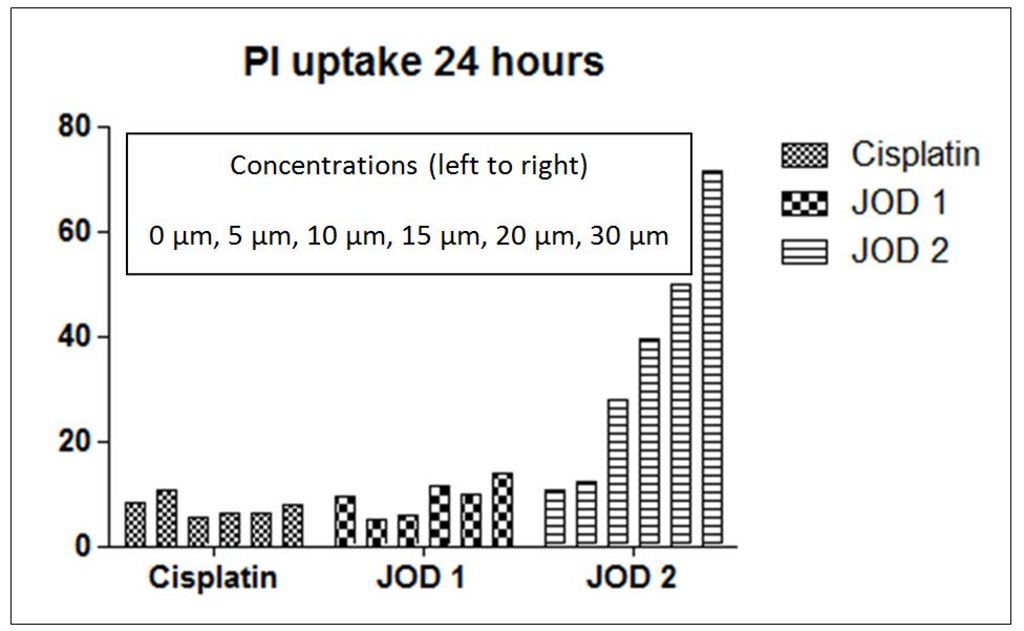
Two of my best candidate drugs were tested by the Cancer Research Facility in UCC under the supervision of professional cancer researchers. In a comparison test on human oesophageal (throat) cancer cells with Cisplatin (the main platinum anti-cancer drug currently on the market), my first drug (JOD1) was taken up (entered the cell) by an equal quantity of cancer cells, compared to Cisplatin. The second drug (JOD2), on the other hand, was taken up by almost four times the amount of cancer cells compared to Cisplatin over the same period of time, 24 hours, at the same concentration.
It can clearly be seen in Figure 2 that the amount of non-viable cancer cells (cells that absorbed the drug) identified after 24 hours for my drug, JOD2, is significantly higher than those identified for Cisplatin. The five bars for each test substance represent progressively higher concentrations of the drug used in each test.
In a comparison of the tested cells after adding the drug it was also confirmed that there were significantly more dead cancer cells after addition of JOD2 than after Cisplatin. The method by which anti-cancer drugs kill the cancer cells is very important in determining whether it will cause side-effects during clinical trials in humans. Type II cell death causes the cell to “burst”, leaving the nucleus behind, which in turn can cause problems later on for patients. Controlled cell death (Type I) is the desired outcome, as it uses the cell’s own mechanisms to destroy itself and leaves very few remaining materials; as a result, this ensures fewer side effects for the patient.
This is one of the first reports in the world of this particular class of platinum-based drugs and the effectiveness of their action against cancer cells through inducing controlled cell death (Type I). This report will almost certainly make an impact on the continued research into further analogues of these drugs across the globe and, hopefully, assist in producing even better platinum anti-cancer drugs in the future.
On-going work
The next step with these drugs is to test for toxicity and confirm that they have fewer side effects than the current drugs available. From the tests already carried out, there are indications that JOD2 should have minimal side-effects in comparison to Cisplatin, but this remains to be confirmed. If these drugs, particularly JOD2, are found to have fewer side effects, then they will go on to be tested on further types of cancers, and eventually clinical trials with human patients.
The potential impact of these drugs on the treatment of certain types of cancer is enormous and, even with the results so far, it seems clear that this new structure of platinum-based anticancer drugs can be very effective against cancer cells by inducing controlled cell death.
I would like to thank my supervisor, Dr. Orla Ni Dhubhghaill, the staff of the Department of Chemistry and all of my colleagues in lab 427 in the Kane Building, University College Cork. I also wish to sincerely thank Tracy O’Donovan and Sharon McKenna in the Cork Cancer Research Centre for their work on testing and reporting the anti-cancer activity of the platinum drugs JOD1 and JOD2 with cancer cells.